Moving towards human clinical trials
Over the past 6 years, Drs. Peter Barry and Alice Tarantal, California National Primate Research Center (CNPRC) at UC Davis, have been collaborating with Dr. Louis Picker at Oregon Health Science University (OHSU)–Oregon NPRC to develop and test a vaccine and potential cure for HIV. OHSU is now recruiting volunteers to be part of the first human trials for this exciting new development in the prevention and treatment of HIV.
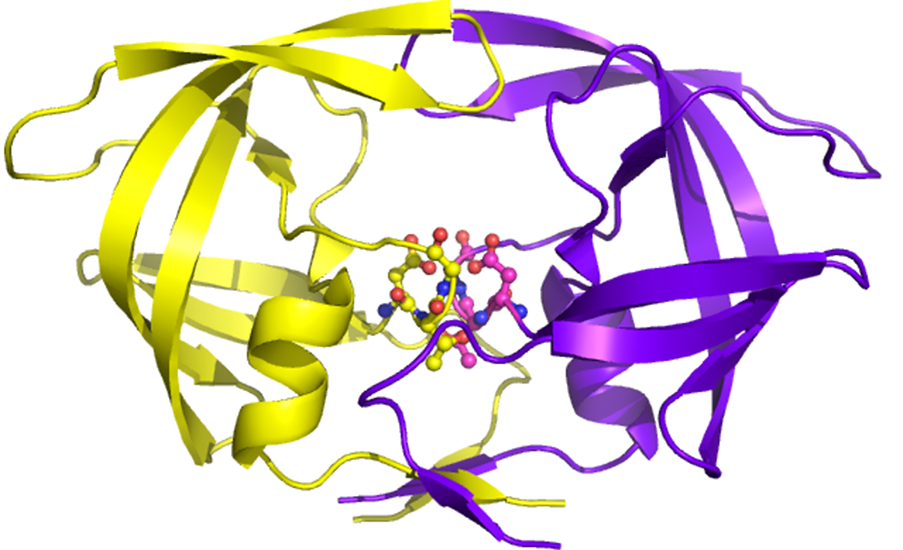
This unique vaccine uses the genetic backbone of cytomegalovirus (CMV), a common virus in humans, to express a small, non-disease causing portion of the HIV virus. CMV is a common strain of Herpes virus that infects up 50-70 percent of adult Americans, but which rarely causes disease symptoms in individuals with a functional immune system.
Peter Barry, PhD, CNPRC Core Scientist and director of the Center of Comparative Medicine (CCM) at UC Davis, is a world-renowned expert in the natural history of the rhesus macaque-specific cytomegalovirus, rhesus CMV (RhCMV). Dr. William Chang, in his laboratory, molecularly engineered the genetic backbone of RhCMV to enable rapid and efficient insertion of non-RhCMV genes that could be expressed as proteins during the course of RhCMV infection. Dr. Barry began his collaboration with Louis Picker, PhD, by supplying him with the engineered RhCMV. Dr. Picker further manipulated the RhCMV genetic backbone into a vaccine vector.
In particular, Dr. Picker was interested in developing a safe HIV vaccine that would generate strong immune responses against HIV infection and disease for the lifetime of the vaccinated individual. Particular attributes of human CMV infection in humans led him to consider human CMV as a novel viral vaccine vector to immunize humans against major infectious disease threats including HIV, tuberculosis, and malaria.
To test his concept, Dr. Picker used the rhesus macaque model of HIV to determine whether such a CMV-based vaccine vector could protect immunized rhesus macaques against virulent simian immunodeficiency virus (SIV) infection, which led to the successful partnership with Dr. Barry to use Drs. Chang and Barry’s modified version of RhCMV.
Dr. Picker’s lab inserted genes of SIV into the RhCMV vector to create a vaccine that trained the immune system to be ready to attack and eliminate SIV-infected cells. The immune system is not naturally trained to fight SIV and is notoriously difficult to control because the immune system doesn’t know to attack it. However, rhesus macaques immunized with Dr. Picker’s vaccine and then exposed to the virus were remarkably protected against SIV infection – more than 50-60 percent were protected. No other SIV vaccine has had that kind of success, either in monkeys or in human trials of HIV vaccines.
At OHSU, Dr. Picker also demonstrated that this novel vaccine mechanism eradicates SIV from the body. Instead of using antibodies to fight the virus, the RhCMV/SIV vaccine stimulates T cells to control and ultimately eradicate SIV infection. Through a mechanism by which no one could have predicted, RhCMV expressing SIV proteins naturally arms CD8+ T cells to be on alert against subsequent SIV. Thus, vaccinating with strains of cytomegalovirus into the body that have been engineered to express particular SIV genes trains the body to attack SIV after exposure.
Dr. Picker and his colleagues are keenly interested in translating the extremely promising results in rhesus macaques to human clinical trials, hopefully beginning in 2017 or 2018. Dr. Picker’s group wants to use versions of human CMV for the human clinical vaccine trials based on the results in the rhesus macaque model. To accomplish this, Dr. Picker is making versions of RhCMV that are further weakened for the ability to cause any disease. Notably, although HCMV is considered a virus with low disease potential, there are some risks associated with primary HCMV infection. Accordingly, Dr. Picker is working with CNPRC and CCM scientists to critically evaluate these new versions for (1) the ability to stimulate immune responses against SIV infection, while (2) exhibiting significantly reduced disease potential.
Drs. Barry and Alice Tarantal, PhD, together with Dr. Yujuan Yue in Dr. Barry’s lab, are actively collaborating with Dr. Picker’s group on safety testing of the weakened versions of RhCMV at the CNPRC in the fetal CMV pathogenesis proof-of-concept model. The results of these critical safety studies are directly informing Dr. Picker’s group on which vectors to use in the human clinical trials.
Research at the CNPRC and ONPRC is supported by the National Institutes of Health, Office of Research Infrastructure Programs, and the Bill and Melinda Gates Foundation.
Related links:
https://cnprc.ucdavis.edu/mother-to-infant-transmission-of-high-risk-infection-new-monkey-model/